Gum Disease - Concord, NH
The Effects of Gum Disease Run Far Deeper Than Your Smile
Schedule ConsultationGum Disease: A “Silent Infection” With Significant Risks
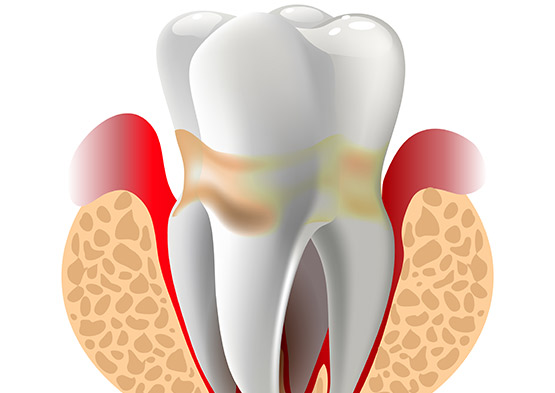
Though common, gum (periodontal) disease is responsible for a number of oral and general health problems. Gum disease is caused by certain types of bacteria. These bacteria produce toxins that result in the loss of bone supporting your teeth. Without treatment, the disease progresses and leads to mobility and tooth loss. Scientists have also observed a link between gum disease and some systemic conditions. Heart disease, stroke, diabetes, dementia, certain cancers, breathing problems and other illnesses may be worsened or brought on by gum disease. Many people are living with gum disease, completely unaware of its presence. It is often considered a silent infection, and may present with or without signs and symptoms.
“Gum disease or periodontitis. Oftentimes when I talk to patients I kind of refer to it as a silent infection because you may have this problem and not even know it.”
Around 75 percent of adults in the United States have some stage of gum disease.
30% or people aged 65–74 have no natural teeth.
Patients with periodontal disease are 2.7 times more likely to experience a heart attack.
The Many Signs and Symptoms of Periodontal Disease
Bleeding. Bad breath. Gum recession. These are common signs and symptoms of gum disease that many patients simply pass off as “normal.” However, bleeding or any other indication of gum disease is never normal, and should be evaluated right away. Treating your gum disease as early as possible is crucial for both your oral and overall health.
Gum Disease Effects Are Irreversible, and Only Worsen Without Treatment
Left untreated, gum disease progresses and bone loss advances. Early treatment and maintenance of gum disease significantly reduces the risk of tooth loss and other problems. Such long-term, irreversible damage often leads to the need for tooth extraction and replacement with a dental implant. Seeking specialized care from Cornerstone Periodontics and Implants offers the best possible outcome when gum disease threatens your smile.